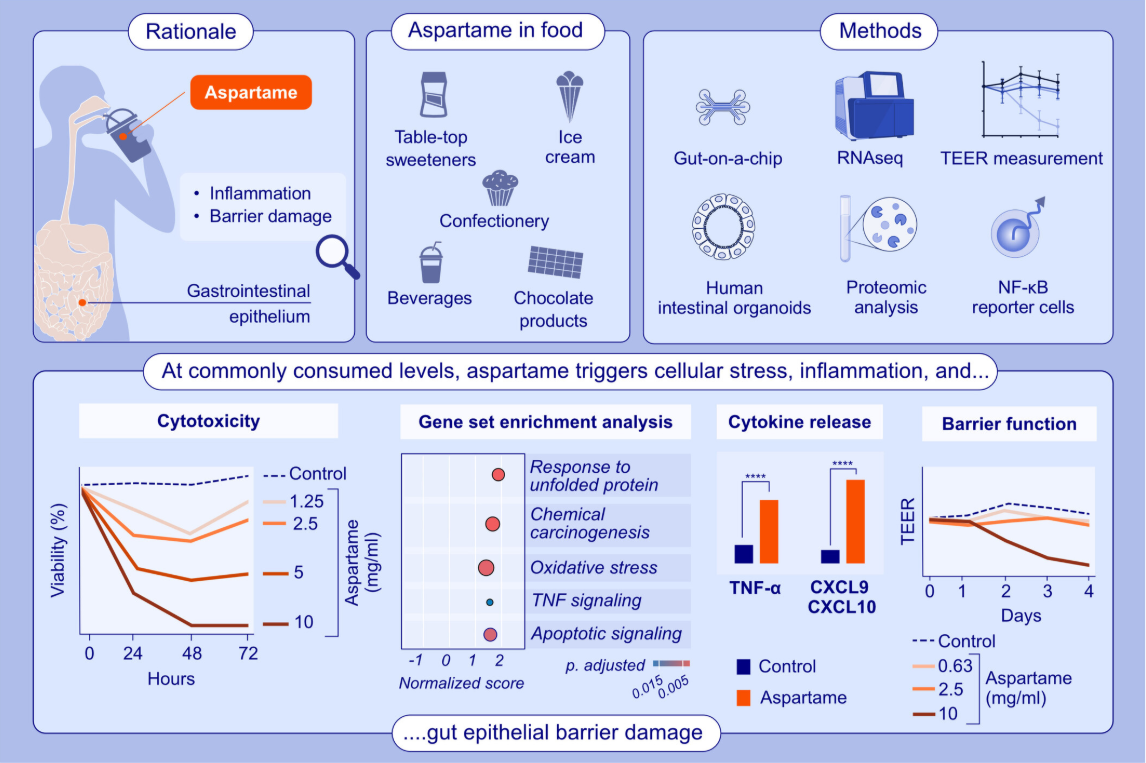
The Epithelial Barrier Theory is a comprehensive explanation for the global, epidemic-level rise in chronic health conditions over the past 65 years. The theory, postulated by Akdis, proposes that exposure to toxic substances introduced by industrialization and modern lifestyle changes disrupts the epithelial barrier of the skin, upper and lower airways, and gut mucosa and causes microbial dysbiosis triggering an inflammatory immune response that can initiate or aggravate more than 70 chronic inflammatory diseases. The Epithelial Barrier Theory includes the ONE HEALTH concept with the strong veterinary medicine involvement of pets and domestic animals.
Learn moreEpithelial Barrier Theory in Lectures
Learn more
The epithelial barrier theory and its associated diseases
Sun N, Ogulur I, Mitamura Y, et al.
Learn more
Epithelial barrier dysfunction and associated diseases in companion animals: Differences and similarities between humans and animals and research needs
Ardicli S, Ardicli O, Yazici D, et al.
Learn more
Epithelial barrier theory in the context of nutrition and environmental exposure in athletes
Kistler W, Villiger M, Villiger B, et al.
Learn more